Tonsillectomy
What do the tonsils do? What happens if they are removed?
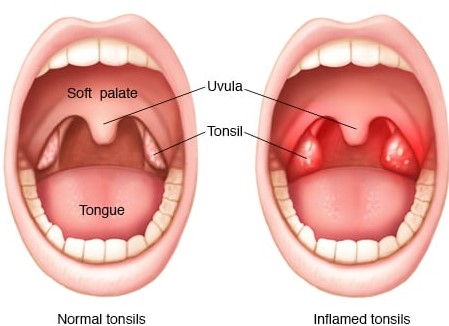
The tonsils are part of your body’s defensive mechanism. They recognize foreign substances that you eat, drink or breathe and communicate with your immune system to defend against infections. It is likely they serve a more important role in the first year of life, however after that, there are so many other sites that detect these foreign substances that the tonsils are no longer essential. Removing the tonsils will make no difference in your body’s ability to protect itself.
Why do we recommend tonsil removal?
Tonsillitis is a common problem. In most people, it only occurs once or twice in a lifetime. In some people however, it can recur often, resulting in multiple courses of antibiotics and time missed from school, work or other commitments.
Currently, we use the “Paradise criteria” as a guide. This criteria is met with 7 episodes of tonsillitis in one year, 5 episodes in two consecutive years or 3 episodes annually in 3 consecutive years. Importantly, there are other reasons for taking the tonsils out in children who do not reach these criteria. If your child meets these criteria or you are concerned about their tonsils you should schedule an appointment to discuss whether a tonsillectomy is the right option for them.
While there are other indications, recurrent infections and tonsil stones are the most common reasons for tonsil removal.
Tonsillectomy explanation video
Post Operative Instructions
Most people take seven to ten days to recover from the surgery. Some may recover more quickly; others can take up to two weeks for a full recovery. The following guidelines are recommended:
Drinking
The most important requirement for recovery is for you to drink plenty of fluids starting immediately after surgery with fluids such as water or apple juice. Some patients experience nausea and vomiting after the surgery. This usually occurs within the first 24 hours and resolves on its own after the effects of anaesthesia wear off. Contact the office if there are signs of dehydration (urination less than 2-3 times a day)
Eating
Generally, there are no food restrictions after surgery, but sometimes a soft diet is better tolerated during the recovery period. The sooner you eat, the quicker the recovery. You may be reluctant to eat because of throat pain; consequently, some weight loss may occur, this is usually gained back after a normal diet is resumed.
Fever
A low-grade fever may be observed the night of the surgery and for a day or two afterward. Contact your GP, Dr Jefferson, or the emergency department if the fever is greater than 38.5º.
Activity
Activity may be increased slowly, with a return to school after normal eating and drinking resumes, pain medication is no longer required, and the child sleeps through the night.
– Travel on airplanes or far away from a medical facility is not recommended for two weeks following surgery
– Swimming is not advised for 2 weeks following surgery.
Breathing
You may notice snoring and mouth breathing due to swelling in the throat. Breathing should return to normal when swelling subsides, 10-14 days after surgery.
Scabs
A white scab will form where the tonsils and adenoids were removed. These scabs are thick and cause bad breath. This is normal. Most scabs fall off in five to ten days after surgery. You may see or taste some blood.
Adenoids
If the adenoids have been removed there may be a foul smell from the nose for up to 2 weeks, please use some FESS nasal spray for kids and use twice per day during this time.
Bleeding
With the exception of small specks of blood from the nose or in the saliva, bright red blood should not be seen. If such bleeding occurs, contact me immediately or go to your closest emergency room.
Pain
Nearly all children undergoing a tonsillectomy/adenoidectomy will have mild to severe pain in the throat after surgery. Some may complain of an earache (so called referred pain) and a few may have pain in the jaw and neck .
Pain control
- A prescription for some oral steroids will be provided on discharge.
Take 1 dose every 48 hours for 3 doses starting three days after your surgery. - Celecoxib is an effective anti-inflammatory, this can be used in preference to ibuprofen (neurofen)
- Patients older than 6 years of age may also get some stronger prescription pain relief.
- Panadol, will be recommended for you on discharge. The pain medication will be in a liquid form but sometimes a rectal suppository will be necessary. Pain medication should be given as prescribed.
Follow up
- On discharge you will get a follow up phonecall from the practice nurse 4-6 weeks after surgery
- If you have any concerns in the meantime, please phone the rooms on (02) 4955 8044.



